Kidney Failure Treatment Without Dialysis
Alternative Approaches to Kidney Failure Treatment without Dialysis
Kidney Failure Treatment Without Dialysis: Exploring Alternative Approaches
Quick Summary
Kidney failure doesn’t always mean dialysis. This article explores alternative treatments including conservative management, kidney transplantation, and emerging medical innovations. Learn how patients can manage kidney failure while preserving their quality of life — without relying solely on dialysis.
Introduction
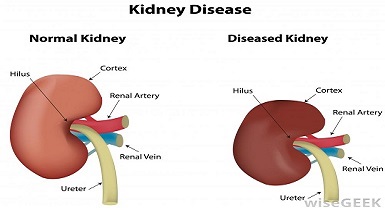
Kidney failure, also known as renal failure or end-stage renal disease (ESRD), occurs when your kidneys can no longer filter waste and excess fluids from the blood effectively. This leads to serious complications such as swelling, fatigue, and a buildup of toxins in the body. While dialysis is a commonly used treatment option, it may not always be suitable for all patients due to medical complications, patient preferences, or limited access to dialysis facilities.
In this article, we will explore Kidney failure treatment without dialysis or non-dialysis treatment options for kidney failure patients, focusing on alternative approaches that aim to manage the condition and improve quality of life without relying on dialysis.
What is Renal Failure?
Renal failure occurs when kidney function declines to the point where the Kidneys can no longer perform essential tasks like filtering waste and regulating fluid balance in the body.
It typically progresses in stages, starting with mild impairment (stage 1) and progressing to severe kidney dysfunction (stage 5, ESRD). At this advanced stage, patients often need renal replacement therapy, such as dialysis or a kidney transplant, to survive.
However, not every patient requires dialysis immediately, and several non-dialysis treatment options can be considered depending on the individual’s stage of kidney disease, overall health, and personal preferences.
Non-Dialysis Treatment Options
1. Conservative Management (Supportive Care)
Conservative management, also referred to as supportive care, aims to optimize the patient’s quality of life by addressing symptoms and slowing the progression of kidney disease. This approach does not involve dialysis or a kidney transplant but focuses on symptom management and maximizing comfort.
Key Components:
- Dietary Modifications: A kidney-friendly diet is crucial. This typically includes controlling protein intake, reducing salt, and limiting phosphorus and potassium-rich foods.
- Blood Pressure and Diabetes Control: Managing hypertension and diabetes is vital to slow down kidney damage. Medications like ACE inhibitors or ARBs can help.
- Fluid and Electrolyte Management: Monitoring fluid intake and balancing electrolytes are key components in preventing complications such as swelling or dangerous imbalances in the body.
- Symptom Management: This may involve using medications to control symptoms like nausea, fatigue, and itching, as well as managing chronic pain or depression associated with kidney failure.
Patient Considerations: Conservative management is particularly suitable for older patients or those with significant comorbidities who may not tolerate dialysis or transplantation.
Research has shown that, in some cases, it may provide a similar or even better quality of life compared to dialysis, particularly for those with a limited life expectancy.
2. Kidney Transplantation: A Non-Dialysis Solution
Kidney transplantation is the gold standard for treating end-stage kidney failure. A successful transplant offers the potential to restore kidney function and free patients from the ongoing burden of dialysis. However, it is not suitable for everyone.
Benefits:
- Improved Quality of Life: Many kidney transplant recipients experience a dramatic improvement in their health and quality of life. They no longer need dialysis and regain energy and mobility.
- Better Survival Rates: Studies show that kidney transplant patients generally have better long-term survival compared to those who stay on dialysis.
Challenges:
- Donor Organ Availability: One of the major hurdles is the limited supply of donor kidneys, making it difficult for many patients to receive a transplant.
- Immunosuppressive Medications: After transplantation, patients need to take immunosuppressants for life to prevent rejection of the transplanted kidney. These medications come with their own risks, such as increased vulnerability to infections and certain cancers.
- Eligibility Criteria: Not all patients are candidates for transplantation, especially those with other serious health conditions or those who are not suitable candidates for surgery.
3. Peritoneal Dialysis (PD): A Home-Based Alternative
Peritoneal dialysis (PD) is a type of renal replacement therapy that uses the patient’s peritoneal membrane as a natural filter to remove waste and excess fluids from the body. Unlike hemodialysis, which requires visits to a clinic, PD can be performed at home.
Benefits of Peritoneal Dialysis:
- Flexibility and Independence: PD can be done at home, offering greater flexibility in daily routines and fewer clinic visits.
- Continuous Treatment: PD offers more gradual and continuous removal of toxins, which can better preserve residual kidney function and reduce the risk of blood pressure fluctuations.
- Fewer Dietary Restrictions: PD patients often have fewer restrictions on their diet compared to those on hemodialysis.
Challenges:
- Risk of Infection: The major complication with PD is the risk of infection, particularly peritonitis, due to the need to insert and remove the dialysis fluid.
- Suitable Peritoneal Membrane: Not all patients have a suitable peritoneal membrane for PD. Some may experience issues with the dialysis fluid not filtering adequately.
Get more insights on Peritoneal Dialysis here by PubMed
Emerging Therapies and Future Directions
The future of kidney failure treatment is bright, with advancements in regenerative medicine, stem cell therapies, and wearable technologies that aim to improve patient outcomes and quality of life.
- Stem Cell Therapy and Tissue Engineering: Research is ongoing into using stem cells to regenerate damaged kidney tissue or create bioartificial kidneys. This could provide patients with a functional kidney without the need for a transplant.
- Wearable Artificial Kidneys: A portable device that mimics the functions of a natural kidney is being developed to provide continuous support to patients. This could revolutionize kidney failure treatment by offering a less intrusive alternative to dialysis.
- Pharmacological Innovations: New drugs are being developed that target inflammation, oxidative stress, and fibrosis, all of which contribute to kidney disease progression. These treatments aim to slow down kidney damage and delay the need for dialysis.
-
SGLT2 Inhibitors: Originally used for diabetes, these medications have shown promise in slowing kidney disease progression.
-
Artificial Kidneys: Development of wearable or implantable devices aims to replicate kidney functions without the need for dialysis.
-
Xenotransplantation: Transplanting genetically modified animal kidneys into humans is under investigation as a potential solution to organ shortages.American Kidney Fund
- iHemo: Intracorporeal Hemodialysis System: The iHemo system represents a groundbreaking advancement in dialysis technology. Developed by The Kidney Project, iHemo is a surgically implanted device that performs hemodialysis within the body, eliminating the need for external blood circulation and needles.
The iHemo system has shown promising results in preclinical studies and aims to provide a safer, more convenient alternative to traditional dialysis methods.
For more detailed information on the iHemo system, read our article: Breakthrough Research in Kidney Failure Treatment Underway at UCSF.
Additional Considerations for Kidney Failure Treatment
Lifestyle Modifications and Diet
Patients with kidney/renal failure can benefit significantly from adjusting their diet and lifestyle. These changes may include:
- Reducing Sodium, Phosphorus, and Potassium: Limiting foods like bananas, tomatoes, and dairy can help manage electrolyte imbalances.
- Fluid Management: It’s essential to control fluid intake to prevent swelling and high blood pressure.
- Exercise: Light exercise, tailored to the patient’s ability, can help maintain physical function and well-being.
- Mental Wellness & Anxiety Management: Managing stress is essential. Chronic kidney disease often brings emotional challenges like anxiety or depression.
Psychosocial Support
Being a patient, I can relate. Kidney failure and its treatments can be emotionally and psychologically challenging. Patients may experience anxiety, depression, or social isolation. Support from healthcare providers, family members, and kidney support groups can be essential in managing these feelings. Cognitive-behavioral therapy (CBT) and counseling can also help patients cope with the emotional strain of the disease.
Meditation, breathing exercises, mindfulness practices, and even cognitive behavioral therapy (CBT) can significantly reduce stress levels and improve overall well-being. Patients are encouraged to explore apps or consult a therapist experienced in chronic illness support.
Tip: Guided meditation Shiv Yog, founded by Dr. Avdhoot Shivanand and furthered by Acharya Ishan Shivanand Ji, offers a transformative approach to holistic healing. Their teachings emphasize the union of body, mind, and spirit, aiming to elevate consciousness and promote self-healing. I myself follow and a part of shiv yog forum. Given me strenth, motivation, healing and preachings of our hindu sanatan dharma.
Costs and Accessibility
Managing kidney failure without dialysis can be cost-effective for some patients, especially when considering the expenses of long-term dialysis. However, kidney transplantation and certain medications can still be expensive. Understanding insurance options, financial aid programs, and the availability of dialysis at home can help patients make informed decisions.
Conclusion
Managing kidney failure treatment without dialysis is a viable option for many patients, especially with treatments such as conservative management, kidney transplantation, and peritoneal dialysis. Each treatment has its pros and cons, and the decision should be tailored to the patient’s medical needs, preferences, and overall health. As research continues to evolve, innovative therapies offer hope for even better outcomes in the future.
Note: It’s essential for patients to work closely with their healthcare providers to determine the best treatment path and understand the emotional, financial, and physical aspects of managing kidney failure.